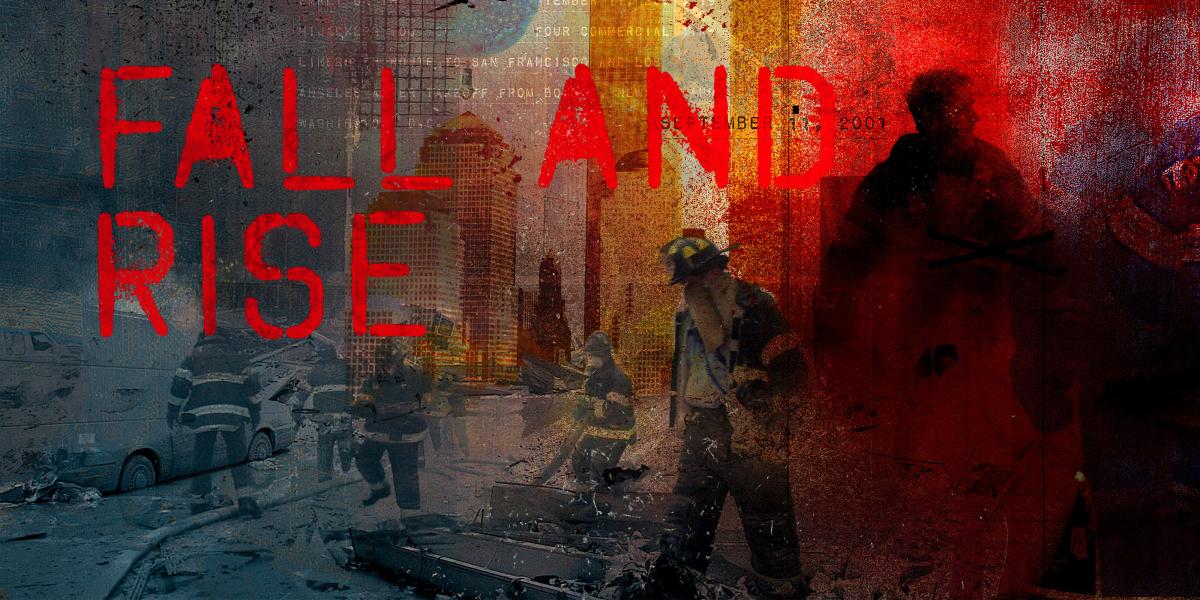
Fall and Rise
A tragic autumn morning in 2001 and a decade’s worth of repercussions for public health
That Was Then
On that Tuesday, on a big screen in the Bloomberg School, Patrick Breysse and Alison Geyh watched as the second World Trade Center (WTC) tower collapsed.
“It hit her right in the heart,” says Breysse, an Environmental Health Sciences (EHS) professor.
“She said, ‘We have to do something.’ I stepped back, let her run, and she took the lead,” Breysse says, recalling the morning of September 11, 2001. Immediately, Geyh, PhD, then an EHS assistant scientist, mobilized a team to travel to ground zero and conduct some of the first environmental health assessments performed at the site.
America’s illusions of safety went up in smoke like the debris burning in lower Manhattan’s pile of rubble. News anchors wept on screen. Military planes patrolled the skies. Civilian flights were shut down. The country had no idea what to expect next.
“Like the rest of the world, the public health community was largely unprepared for this kind of event,” says Thomas Burke, PhD, MPH, now associate dean for Public Health Practice and Training at the School.
Alfred Sommer, MD, MHS ‘73, then dean of the School, had been literally out to sea during the attacks, aboard the Queen Elizabeth II. He returned to find his faculty stunned but eager to marshal resources. “[Tom Burke] was with me when it hit me,” he recalls. “The School has to organize itself as an institution critical to the acute problems requiring public health.”
“I vividly remember watching them pull a torso out of the pile. There was a teddy bear in the rubble. I thought, ‘These are the remains of private lives. Part of that dust is human remains. We’re breathing people.’” —Patrick Breysse
With colleagues, Burke began to organize faculty teams with the primary mission of training and education in preparation for threats. Locally, he reached out to public officials and developed relationships with the Baltimore Mayor’s Office, the police force and firefighters.
Then, on October 2, 2001, terror struck again. A photo editor at The Sun, a supermarket tabloid in Florida, was diagnosed with anthrax. By October 17, two senators had been targeted and 31 Capitol workers had been diagnosed with anthrax. Once again, the School and the nation went on high alert. This time for bioterrorism. “[But] by the time of anthrax,” says Burke, “we had a network in the School… For the first time, first responders and police were working with public health practice [professionals].”
Meanwhile, in New York City, Geyh, Breysse and a team of students had brought equipment to ground zero. Arriving in late September, Geyh managed to get permission for her team to work on the site, a herculean task at the time. The challenges seemed insurmountable—jurisdictions changed constantly, bureaucracy was steep, and there was no coordination among the countless people, agencies, universities and medical services that converged to help. “No one was really willing to step up,” says D’Ann Williams, a student at the time, “and Alison did.”
Geyh secured entree by collaborating with an industrial hygienist with the International Brotherhood of Teamsters’ Safety and Health Department; the Teamsters represented the truck drivers who drove away the debris. Her team expanded their efforts to include ironworkers (who cut the enormous debris), crane operators, carpenters, laborers and dock builders, each with their own unions that, unlike the firefighters and police unions, did not have built-in health services. Says Julie Herbstman, who was on Geyh’s team and is now an assistant professor at the Columbia Mailman School of Public Health, “The trade unions were major players at the site but didn’t have anyone looking out for them.”
“We were some of the first people on the site doing air sampling,” says Breysse, PhD ’85, MHS.
Their team performed respiratory health and exposure assessments for the truck drivers and others. Herbstman, PhD, ScM, and Williams, DrPH ’10, MS, now an EHS research associate, helped characterize the airborne particulate matter, asbestos and volatile organic compounds at the perimeter and in the middle of the site. Their findings helped to justify medical monitoring that continues today.
“[The Baltimore City health commissioner] called and asked if I would help with preparedness for radiation, dirty bombs, things like that. I said, ‘Sure, whatever you need.’ Then I hung up and Googled ‘dirty bomb.’” —Jon Links
Geyh’s team returned in December 2001, and again in April 2002, and they’ve published several studies addressing health effects of the plume that hung over Manhattan. One finding identifies short-term health effects, which include respiratory and musculoskeletal problems, eye injuries and elevated rates of post-traumatic stress disorder, anxiety and depression among rescue and recovery workers and volunteers. Some firefighters at the site developed the “World Trade Center cough,” and exposure was associated with a substantial and “probably permanent” loss of lung function, according to Geyh and her co-authors.
While the short-term effects have been documented, both Breysse and Burke note that people working at the site were exposed to inhaled carcinogens—and they acknowledge that any associated increased risk for types of cancer may not become apparent for decades.
“The problem with emergency response situations is that you often don’t recognize there’s a health problem until time has passed,” says Breysse. “The big mistake with the 9/11 response was what happened to the workers on the site. We’ve learned from what happened after 9/11 to pay more attention to health and safety of responders.”
This Is Now
In February of this year, at the age of 52, Geyh died of cancer. It’s impossible to connect her cancer to her work at the site; as Burke points out, “One-fourth of us will die of cancer.” At her memorial, two Teamsters sang her praises; her research may assist with the diagnoses of future work-related respiratory illnesses. “It’s the saddest thing that you can’t talk to Alison,” says Herbstman. “She provided a huge service to the labor unions and to research.”
So what has been learned since 2001? Is public health better prepared now to cope with emergencies and disasters in the wake of 9/11? Some public health advocates say great strides have been made in some areas—but they note there is still much to be done.
Nationwide and locally, over several years, Jonathan Links, PhD ’83, an EHS professor, conducted surveys that explored the willingness of public health officials to respond in emergencies, such as natural disasters or outbreaks.
“There’s been a profound cultural shift. It took seven or eight years, but now public health professionals think of themselves as first responders… Public health has gone from 9-to-5 to 24/7.” —Jon Links
“[In] those first studies in Maryland [in 2005], about half of the workers were not willing to respond… However, one of the main factors driving that unwillingness is a perception that their role in their health department’s response isn’t important, and they are wrong about that! The person who answers the telephone is profoundly important in an emergency.” Subsequent training by Links and colleagues has helped to get public health workers to think of themselves as first responders.
Burke, who is director of the Johns Hopkins Risk Sciences and Public Policy Institute, has gone on to create a preparedness curriculum. And there is now a doctoral track in risk assessment. Links developed the School’s pandemic flu plan and subsequently worked with the Johns Hopkins Office of Critical Event Preparedness and Response (CEPAR), of which he is now deputy director. He also directs the School’s CDC-funded Public Health Preparedness Programs, which are doing a combination of research (including work on first-responder attitudes about willingness to report for duty, and how to enhance willingness), training and technical assistance to local health departments.
Ten years later, the health impact of 9/11 is still being measured. A paper co-authored by Geyh in 2007 argues, “Still, there are some things we will never know for certain; indeed, we do not even know with any certainty the size of the exposed population.” A further wrinkle is the problem of association. Adds Herbstman: “We can measure biomarkers to see who had highest exposures to what, but we can’t say with confidence the exposures are due to WTC.”
With Hurricane Katrina, H5N1, H1N1 and the Gulf oil spill, the need for strong public health preparedness has been confirmed and reconfirmed. Perhaps because of lessons learned in the wake of 9/11, faculty at the School were faster and better at responding to some of these events.
“In the Gulf oil spill,” says Breysse, “BP paid attention to worker protection. They collected air samples, they did a lot more environmental sampling—that’s a result of 9/11. Now we’re thinking ahead of the game.”
Of the funding that followed 9/11, Sommer says, “It took years for funds to be distributed into the vaccine industry, and we still have no capacity.”
Overall, he is skeptical about how much progress has been made. “We’re a disorganized society,” he says. “I don’t think we’ve gone anywhere, really. Look at how we responded to Katrina. Perhaps we’re better at identifying a threat, such as SARS or flu. But do we have new drugs for anthrax? No. Do we have new vaccines for anthrax? No. Do we have new ways to deliver vaccines in an organized manner? No.”
“We haven’t gone far… I bet very few faculty have adequate emergency drinking water. I bet very few people have adequate food supplies… The country may have let its guard down.” —Thomas Burke
Says Links, “[As a country] our risk communication is still terrible… We do an absolutely terrible job of getting the public prepared. I think we’ll finally achieve what we need to achieve when preparedness and response are viewed as a natural part of public health activities.”
Burke is encouraged by the increase in students taking courses in preparedness: “I think we have made progress and our students are more dedicated than ever to making a difference and making sure we can be ready to respond to the threats of the future.