A Shower Cap EEG in Bhutan
When a school kid in just about any developing country has an epileptic seizure, chances are that fellow students and even teachers will shy away instead of trying to help.
Tenacious superstitions that epilepsy sufferers are either possessed or contagious surround this disease, which afflicts 65 million worldwide.
Of that number, almost 90 percent live in developing countries where causal factors are not addressed and cases remain severely under- and misdiagnosed despite effective and available and relatively affordable treatment.
“This is a disorder of children, youth and working-age adults mostly, and when there is inadequate diagnosis and limited treatment, the cost to society is potentially very high,” says Farrah Mateen, MD, PhD ’14, who started working in the Kingdom of Bhutan in 2009. She has been back several times and plans to go again
Mateen is focused on interventions and low-cost diagnostics for brain disorders with the goal of facilitating a “technological leap” in resource-limited settings. Along with doctoral studies at the Bloomberg School, Mateen simultaneously completed a fellowship in the Division of Neuroimmunology and Neurological Infections at the Johns Hopkins School of Medicine. “This training allowed me to develop clinical expertise with vulnerable populations in Baltimore and abroad,” she says.
Now a neurologist and faculty member at Massachusetts General Hospital of Harvard Medical School, and the University of Ottawa, Mateen is conducting a clinical trial in Bhutan to test a low-cost mobile electroencephalography (EEG) device that could become a routine tool in developing countries for the diagnosis of people with seizure disorders. There are an estimated 10,000 cases of epilepsy in Bhutan.
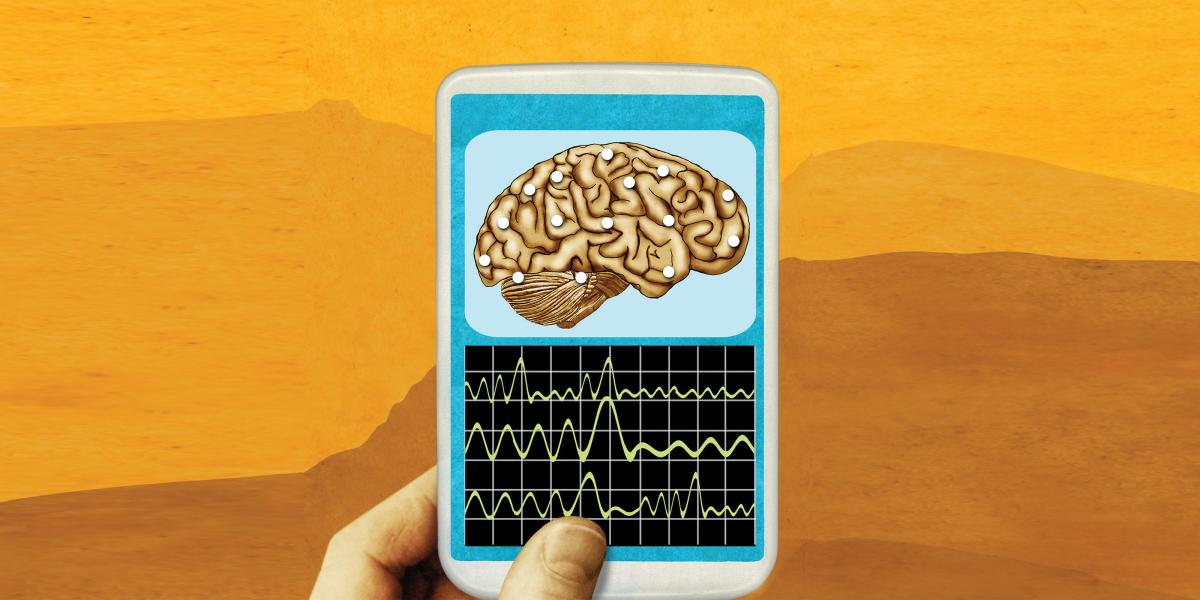
The device takes the form of a “shower cap,” with roughly a dozen leads that are attached to a patient’s scalp for 20–30 minutes to monitor the brain’s electrical signals. The signals are fed into a smartphone app that records the EEG.
Health care workers who give the test don’t require formal medical training, and the data are easily transmitted for expert interpretation. That’s helpful in a country like Bhutan, which has not a single neurologist and just one non-functioning, stationary EEG machine at the main hospital in the capital Thimphu, days of walking away for many of the country’s 900,000 citizens.
The device, operating on open software developed at the Technical University of Denmark, costs $275, compared to approximately $15,000 for current stationary EEGs. The work is funded by Grand Challenges Canada, which rewards technological innovations in projects with other social and economic benefits, as well as the Thrasher Foundation.
Mobile technologies particularly benefit young children who can suffer small, non-violent seizures that might be mistaken for staring spells, according to Mateen.
Once a diagnosis of epilepsy is made, doctors can then prescribe a medication. The government of Bhutan provides anti-epileptic drugs free of charge.
This technology has the potential to improve the diagnosis of epilepsy in other developing countries, including in Africa where a dozen countries with a combined population of 26 million lack a neurologist, and 23 other countries have four or fewer neurologists.
“Populating the world with neurologists, which involves training of a decade or more, is impossible, but we can roll out technology that is cheap and simple to use,” says Mateen.