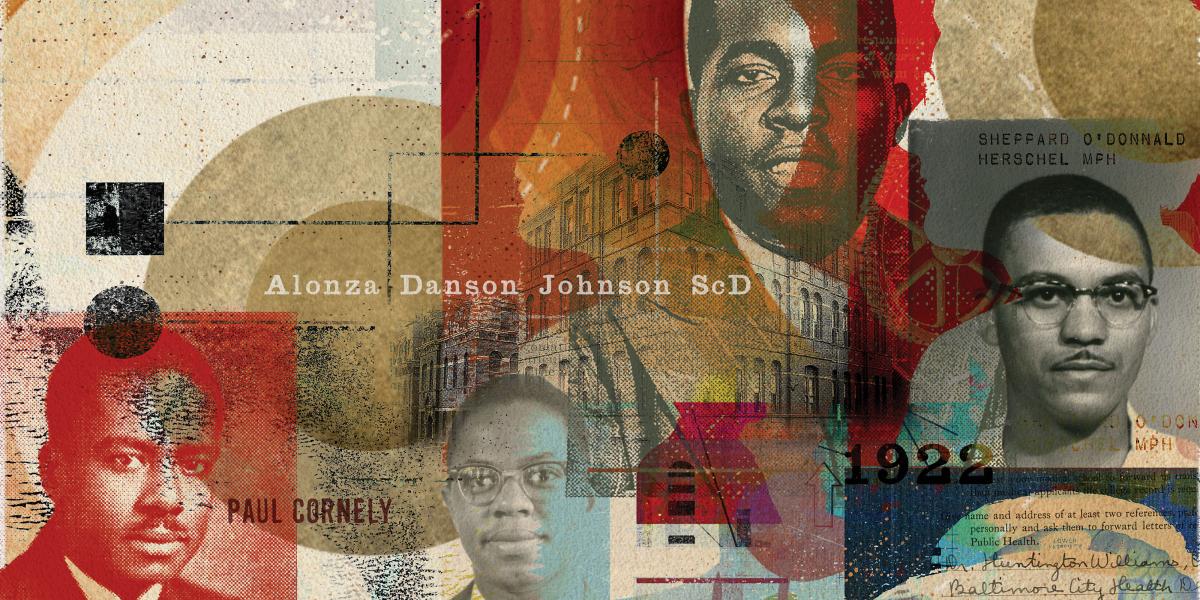
The Color Line, Broken
How segregated admissions at Johns Hopkins finally ended.
In 1922, Barnett M. Rhetta, MD, began applying for graduate study in public health at Johns Hopkins. As president of the Monumental City Medical Society and chairman of the Baltimore Interracial Commission, he was an excellent candidate.
But the Black physician ran into a menacing obstacle: prejudice.
Because Johns Hopkins was private and had one of the nation’s few graduate schools of public health, the University represented his best chance for admission. Maryland’s racial segregation laws barred Black residents from attending white public universities and relegated them to Black colleges, which had inferior funding, libraries, and research facilities. And no Black school in Maryland offered graduate or professional degrees.
From its inception in 1916, the School had admitted a multiethnic student body that included physicians from Latin America, Europe, and East and South Asia. But for the next three decades, Johns Hopkins remained firmly closed to Blacks. If they wanted to pursue advanced education, they would have to leave Maryland.
Rhetta saw glimmers of hope on the horizon when the University of Michigan became the first U.S. school of public health to admit a Black student, Paul Cornely, who earned a DrPH in 1934. (Cornely would go on to become the APHA’s first Black president in 1968.) In 1936, Baltimore’s own Thurgood Marshall, on behalf of the National Association for the Advancement of Colored People Legal Defense Fund, won a key lawsuit, Murray v. Maryland. In its ruling, the court ordered the University of Maryland Law School to admit the Black plaintiff, which ushered in the desegregation of graduate and professional education at white Southern public universities.

Rhetta wrote to Johns Hopkins President Isaiah Bowman in April 1938. He noted that the Harvard School of Public Health had just accepted a Black Baltimore physician, H. Maceo Williams, to its Master of Public Health program. Johns Hopkins should follow suit, Rhetta argued. But 16 years after beginning his quest to be a graduate public health student at Hopkins, Rhetta would be blocked again. His efforts lobbying for admission were rebuffed by Bowman, who was openly segregationist and anti-Semitic, as well as by two public health deans who were sons of Confederate generals. Wade Hampton Frost, dean from 1931 to 1934, was named for Wade Hampton, the Confederate brigadier general under whom Frost’s father had served in the Civil War. During Reconstruction, a paramilitary group, the Red Shirts, helped elect Hampton governor of South Carolina by disrupting elections and brutally intimidating and even murdering Black voters. Allen W. Freeman, dean from 1934 to 1937, was the son of General Walker Buford Freeman, the honorary commander-in-chief of the United Confederate Veterans. Freeman’s brother, Douglas Southall Freeman, authored the definitive multivolume biography of Robert E. Lee. President Bowman and the two deans were disinclined to challenge Johns Hopkins’ whites-only admissions policy for U.S. students.
The School’s governing body, the Advisory Board, was no help, either. Under an existing agreement with the health department, the School had previously admitted white, health department physicians tuition-free. But the Advisory Board rejected a request from Baltimore City Health Commissioner Huntington Williams, MD, DrPH ’22 (who wrote Maceo Williams’s recommendation letter for Harvard) to accept four other Black physicians to the MPH program. The Advisory Board routinely turned to a dubious legal excuse to justify rejecting Black applicants: Since the Maryland General Assembly made a small annual payment to Johns Hopkins, the University was a state-supported institution obliged to follow segregation laws. In fact, private universities such as Johns Hopkins were free to determine their own admissions policies. For example, Black graduate students attended American University and the Catholic University of America in nearby Washington, D.C. The Advisory Board even rejected an application from a Black physician preparing for service in the Ethiopian Ministry of Health. (The only exception was in 1933, when Marjorie A. Forte and Myrtle M. Patton, Maryland’s only two Black public health nurses, joined 50 white nurses at a one-day Institute of Hygiene hosted by the School.)
Then in November 1938, the U.S. Supreme Court ruled in Missouri v. Gaines that the constitutionality of segregation laws rested “wholly upon the equality of the privileges which the laws give to the separated groups within the State.” If none of a state’s public universities would admit Blacks to graduate and professional programs offered to whites, then the state government would be obliged to build new separate schools for Blacks that were demonstrably equal to those for whites. The Gaines decision prompted one member of the all-white Johns Hopkins faculty, political science professor Broadus Mitchell, to mount a public critique of the University’s segregationist admissions policy. Citing the racial disparity in Baltimore’s mortality rates, Mitchell charged that by excluding Black students, Johns Hopkins was “turning our backs on the part of the population that needs us most.” He took aim at the School of Hygiene’s international reputation to reinforce his point. “The Caroline Islands have our solicitude before Caroline Street Baltimore,” he declared, “and the Dutch East Indies before Druid Hill Avenue.”
Soon after Missouri v. Gaines, Maceo Williams returned to Baltimore with his Harvard graduate degree and became the first African American doctor on the Baltimore health department’s full-time staff. From 1939 to 1966, he served as the founding director of the Druid Hill Health Center in West Baltimore, the city’s first neighborhood clinic for Black patients. Among his first tasks was to assist the School in obtaining the cooperation of Black East Baltimore residents for a major public health survey in 1939. The move to bring Maceo Williams on the health department’s staff was part of a larger national movement to address Black health needs in response to the growing influence of the medical civil rights movement. In the segregated South, the U.S. Public Health Service partnered with health departments to enlist Black doctors, nurses, and laypeople to extend public health programs into the Black community under the slogan “germs know no color line.” However, Baltimore’s health department still would not allow a Black physician to treat white patients. Similarly, white-run Southern hospitals, including Johns Hopkins Hospital, prevented Black doctors from entering residency programs or obtain admitting rights—even to care for Black patients in separate Jim Crow wards.
When healthy soldiers became a national defense priority, the color line at Johns Hopkins would finally break. After the U.S. entered World War II in December 1941, news of high rates of syphilis among recruits revived fears from World War I that sexually transmitted infections, then called venereal diseases, or VD, would impede the fighting effectiveness of the armed forces. With manpower at a premium, the War Department assigned VD control officers to all major Army detachments, and Johns Hopkins stepped in to supply trained physicians. Under this program, the School of Hygiene admitted its first African American student, Reginald G. James, MD, MPH ’46, who enrolled in fall of 1945. James, a PHS officer and Rockefeller Foundation fellow, had assisted the Alabama State Health Department in its VD survey and treatment program in rural Macon County, the home of Tuskegee Institute. James succeeded where previous qualified Black applicants had failed because the PHS and the School considered him a strategically valuable partner in the campaign against syphilis among Blacks in the military and across the South.
The School began admitting African Americans to all its degree programs, but the University did not admit Black nursing students until 1952 or medical students until 1963. Despite the School’s international diversity during this era, by 1961, it had awarded degrees to only five Black men and one Black woman. Before 1970, the only U.S. school that produced significant numbers of African American public health graduates was North Carolina College, a Black state school that, in partnership with the University of North Carolina School of Public Health, awarded more than 100 bachelor’s degrees to health educators.
James earned his MPH in 1946, becoming the first Black graduate of Johns Hopkins University. He served as a career PHS officer. As a member of the U.S. Department of Health, Education, and Welfare’s Ad Hoc Advisory Panel on the Tuskegee Study, James was among those who, in 1973, declared the infamous Tuskegee syphilis study (the longest nontherapeutic medical study in U.S. history) “ethically unjustified.” The national outcry over the Tuskegee Study led to the development and implementation of modern human subjects research protections, including the establishing of institutional review boards.